- 3 months ago
- 13Minutes
- 4098Words
- 3172Views
Understanding IBS
(3) Intestinal permeability–a new target for disease prevention and therapy. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/25407511?dopt=Abstract&holding=npg
(4) Association of symptoms with gastrointestinal microbiota in irritable bowel syndrome. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/20857523?dopt=Abstract&holding=npg
(5) Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/18824556?dopt=Abstract&holding=npg(6) Diet rapidly and reproducibly alters the human gut microbiome. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/24336217?dopt=Abstract&holding=npg
(7) Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/21691341?dopt=Abstract&holding=npg
(8) Functional GI disorders: from animal models to drug development. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/17965064?dopt=Abstract&holding=npg
(10) Stress system–organization, physiology, and immunoregulation. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/17709947?dopt=Abstract&holding=npg
(11) Brain-gut microbiome interactions and functional bowel disorders. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/24583088?dopt=Abstract&holding=npg
(12) A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/19337833?dopt=Abstract&holding=npg
(13) Review article: dietary fibre–microbiota interactions. PUBMED http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4949558/
(14) The impact of gut microbiota on brain and behavior: implications for psychiatry. PUBMED http://www.ncbi.nlm.nih.gov/pubmed/26372511
(15) Gut Microbiota and Inflammation. PUBMED http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257638/
(16) Think Twice: How the Gut’s “Second Brain” Influences Mood and Well-Being. The Scientific American http://www.scientificamerican.com/article/gut-second-brain/
(17) Prevalence and impact of self-reported irritable bowel symptoms in the general population. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6498809/What Is IBS?
Irritable bowel syndrome (IBS) is one of the most common and most annoying, painful problems in modern society. If you suffer from it then you will have found little long-term help from your doctor and it can be years before there is any solution, if at all. This is because the causes are very complex, poorly understood, and difficult to treat with conventional drugs.
In this article, I’m going to briefly outline the symptoms, statistics, and proposed causes, then provide you with some potential natural solutions.
IBS SYMPTOMS
Diagnostic criteria for irritable bowel syndrome (IBS) include recurrent abdominal pain or discomfort at least 3 days per month in the past 3 months associated with two or more of the following:
- Improvement (Pain reduction) with defecation;
- Onset associated with a change in the frequency of stool;
- Onset associated with a change in the form (appearance) of stool; and/or
- Criteria fulfilled for the past 3 months with symptom onset at least 6 months before diagnosis.
Discomfort means an uncomfortable sensation not described as pain. During screening evaluation, pain or discomfort frequency must be at least 2 days per week to qualify subjects for clinical trials. (1)
It is well established that Irritable Bowel Syndrome (IBS) symptoms give feelings of shame, fearfulness, and embarrassment, while patients also report being misunderstood by their doctors, their family members, and friends. (12)

IBS STATISTICS
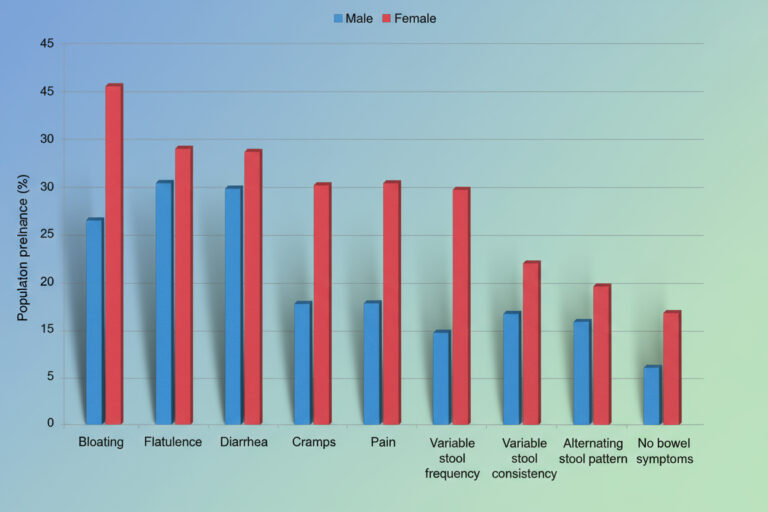
You can see in this chart just how common the symptoms of IBS are in the general population. (17)
To highlight just a few of these countries:
- 15-19% of New Zealanders,
- 10-14% of British, and
- 5-9% of Americans and Australians are affected.
It is interesting how less than 5% of Chinese and Indian people have IBS while Mexicans are over 30%.
The obvious question here is has this got something to do with local dietary habits?
POTENTIAL CAUSES OF IRRITABLE BOWEL SYNDROME
Although the cause of irritable bowel syndrome (IBS) has not yet been completely understood, multiple factors appear to have a role, including:
- The composition of the gut microflora,
- Intestinal permeability,
- Immune response, and
- The gut-brain connection.
I will discuss each one of these breifly below.
Gut Microbiome And IBS
The gastrointestinal microflora is a vast and diverse ecosystem inhabiting the entire digestive tract, with a systemic influence on human health.
Research findings:
- Associations have been observed between patients’ self-reported IBS symptoms and the presence or absence of specific gut bacteria.
- Several bacterial strains were found to be significantly reduced in IBS subjects compared to healthy controls. (4)
Dietary influence on gut flora:
- Microflora activity reflects differences between herbivorous and carnivorous diets, balancing carbohydrate fermentation and protein fermentation.
- Foodborne microbes from both plant- and animal-based diets can transiently colonize the gut, including bacteria, fungi, and viruses.
- These results show the gut microbiome adapts rapidly to dietary changes. (6)
Imbalances in the gut microbiome:
- Disruption of intestinal microflora — or the overgrowth of unwanted fungi, bacteria, and viruses — can damage the sensitive gut mucous membrane.
- This disruption is linked to common IBS symptoms such as bloating, abdominal pain, and irregular bowel movements.
Restoring gut balance:
Probiotics (beneficial live bacteria) and prebiotics (fibers that feed healthy bacteria) play a major role in:
- Rebuilding a healthy gut microbiome.
- Supporting intestinal barrier function.
Reducing symptoms of irritable bowel syndrome (IBS).
Read More About Probiotics and Prebiotics Here
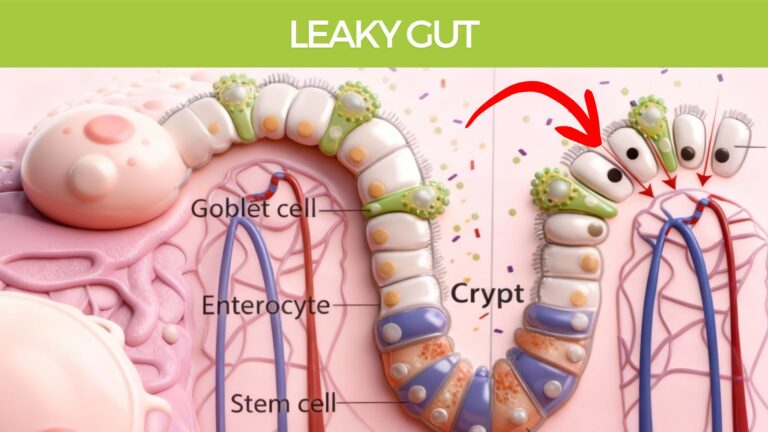
Intestinal Permeability & Leaky Gut
The intestinal barrier has two key roles:
- Protecting the body from harmful microorganisms and toxins.
- Allowing absorption of essential nutrients, fluids, and electrolytes.
- This balance is achieved through complex anatomy and physiology. The barrier represents a large mucosal surface where billions of gut bacteria interact with the body’s largest immune system. (3)
IBS and leaky gut connection:
- A study found colon tissue samples had significantly higher permeability in IBS patients compared to healthy subjects. (5)
- This supports the link between leaky gut syndrome and irritable bowel syndrome (IBS).
Underlying causes of Leaky Gut in IBS:
Disturbances to the gut microbiome may trigger an inflammatory immune response.
This leads to:
- Gut wall inflammation.
- Increased intestinal permeability.
- Entry of toxins, bacteria, and pathogens into the bloodstream.
Gut barrier function:
- Plays a crucial role in preventing unnecessary inflammatory reactions to the microflora. (3)
- Regulated by a finely tuned network of immune mechanisms.
- Because increased permeability and inflammation are linked, natural strategies that reduce gut inflammation are highly beneficial for IBS.
Triggers for inflammation:
- Inflammation arises when bacteria, fungi, or viruses move into places they don’t belong.
- Key differences from human cells include:
- Bacteria and fungi have cell walls.
- Viruses carry unique DNA and RNA structures.
- The immune system immediately detects these as danger signals, triggering inflammation. (15)

Immune Response And IBS
Infectious gastroenteritis is the strongest known risk factor for the later development of irritable bowel syndrome (IBS).
Higher IBS symptom rates have also been observed in:
- Patients with inflammatory bowel disease (IBD), even during remission.
- Patients with celiac disease, despite following a strict gluten-free diet.
Immune system changes in IBS:
Research shows an increased number of immune cells in both the small and large intestines of IBS patients.
This suggests IBS may involve ongoing immune activation and low-grade inflammation. (2)
Natural support strategies:
Supporting both the immune system and the gut microbiome can help:
- Improve overall digestive function.
- Reduce gut inflammation.
- Alleviate IBS symptoms naturally.
The Gut-Brain Connection And IBS
The gut, brain, microbiome, and immune system are in constant two-way communication during both health and disease.
The “second brain” – Enteric Nervous System (ENS):
- Technically called the enteric nervous system, this network consists of sheaths of neurons embedded in the gut wall, extending from the esophagus to the anus (approx. 9 meters).
- The ENS contains 100 million neurons, more than in the spinal cord or peripheral nervous system. (16)
Brain influence on gut function:
The brain, via the nervous system, regulates:
- Intestinal motility and fluid secretion. (8)
- Intestinal permeability. (3)
- Immune function. (10)
- Gut microflora composition. (11)
All of these mechanisms are often dysregulated in IBS.
Emotional and mental health link:
- The connection between stress, emotions, and digestion is powerful.
- Mental and emotional wellbeing must be considered in the management of IBS symptoms.
Neurotransmitters in the gut:
- The enteric nervous system uses 30+ neurotransmitters, similar to the brain.
- Remarkably, 95% of the body’s serotonin is located in the gut.
- In IBS, excess serotonin activity in the gut may contribute to symptoms — leading some researchers to describe IBS as a “mental illness of the second brain.” (16)

The Pharmaceutical Approach
The most commonly prescribed drugs for IBS include laxatives, antibiotics, antidiarrhoeals, and anti-depressants.
All of these drugs may provide some temporary relief of symptoms but none offer a long-term solution by way of treating the cause of the problem. The underlying dietary habits, general gut health, and mental status may not have been resolved. This is where natural, holistic, healing and preventative solutions come into their own.
IBS NATURAL SOLUTIONS
When looking at a complex multi-faceted problem like IBS conventional treatments often work short-term but fail to provide long-term relief. This is because the problem can be subtle and lie largely within the realm of dietary, nutritional emotional, and mental systems.
The areas of gut microflora, intestinal permeability, immune response, and gut-brain connection all fall into strong categories for natural solutions.
Let’s look at each of these individually

Irritable Bowel Syndrome Diet
There are a lot of theories on dietary advice for IBS but nothing that is conclusive or that can be applied to everybody.
Some things seem fairly obvious when you look at the research. Inflammatory foods, lack of pre-biotic containing fruits and vegetables, and low fiber intake must all be factors.
Foods to Avoid
Irritating food for the digestive system includes the following:
Red Meats – Highly acid-forming and inflammatory
Added Sugar – Highly detrimental to gut health
Processed foods in general (including pasta)
Processed grains especially wheat, and other products containing gluten, pasta, pastry, cake, etc.
Too many high-lectin nuts and legumes like baked beans, chickpeas, and lentils. Read more about Lectins Here.
Gas-forming foods – Raw cabbage, cauliflower, broccoli. Read more about Bloating and Gas Here.
Plus don’t follow a raw food salad diet until the IBS symptoms have gone
Recommended foods
Eat plenty of fruit and vegetables (try stewed apples)
Cooked root vegetables (except potatoes)
Vegetable Soups, mushroom, pumpkin, parsnip
Chicken and fish (instead of red meats)
Probiotic drinks and yogurt smoothies
Digestive herbs and mild-medium spices especially turmeric, mint, cinnamon, rosemary
Black tea and herbal teas inclduing peppermint, ginger, and chamomile. Buy Herbal Teas Here
- Mild Curry’s are also recommended, as they contain many if the digestive supporting herbs and spices.

Immune Regulation for IBS
The intestinal immune system has developed a tightly regulated control to optimize the protection against pathogens, while at the same time avoiding unnecessary immune activity. (15)
Supporting the entire immune system along with prebiotics and probiotics will be the best approach.
You can use foods to do this:
Mushrooms – which boost our immunity;
Garlic – high in sulfur which boosts immunity;
- Onions – and Leeks, are anti-inflammatory
Vitamin C foods – anything fresh will contain Vitamin C;
Aloe Vera juice – 50ml daily.
For a selection of ideal recipes Click Here and Choose ‘Irritable Bowel Syndrome’ for the ‘Special Diet’ Selector.

The Ultimate Herbal IBS Program
I have put together a combination of herbs the soothe the gut wall, reduce inflammation, restore the gut microbiome, and clear the system of toxins, regulating the immune response.
Below we explore each of the remedies and how it contribugtes to the resolution if irritable bowel syndrome.
Aloe Vera For Healing The Gut Wall
There there’s nothing I have found better for healing the gut wall over the long term than Aloe Vera Juice. You will find it mentioned further below, but it’s worth looking at it and a little more detail if you’re really interested. Aloe Vera has an amazing power to heal tissues and has a great reputation for speeding recovery from Burns and other tissue damage. Science doesn’t fully understand how it works yet, as it has over 200 active components in the Aloe Gel. I personally recommend this hello vera gel which has no additives or preservatives, or you could grow yours at home and make it yourself. Watch this video if you want to try that.
DOSE: Take 30ml daily first thing in the morning on an empty stomach.
Gut Microbiome For IBS
I suggest using the powerful Human prebiotic strain L-Reuteri, which you can get in the product called BioGaia. Take 2 tablets daily for the first month and 1 tablet daily for the second month. Click here to find out more.
DOSE: Take 1 tablet with water just before Dinner

Herbal Tea For Irritable Bowel Syndrome
Herbal Teas to reduce inflammation and intestinal permeability:
- Raspberry
- Peppermint
- Chamomile
- Ginger
Try a mixture of these teas in your teapot and drink 2-3 cups daily. You can get this blend pre-made here. You will just need to add some fresh ginger.
DOSE: Take 2-3 cups daily from a teapot, great in the evening.

Liver & Bowel Detoxification for Irritable Bowel Syndrome
Some of the anti-inflammatory herbs traditionally used to encourage healthy microflora, heal the gut wall, and reduce negative bacteria and parasites include the following herbs, all of which are contained in the BodiClenz formulation.
One of the most effective things I have seen help with irritable bowel syndrome is the 14-day herbal Bodicleanz program. It contains a combination of 24 herbs designed to support bowel health and digestive processes. You simply take the powder twice a day and a smoothie for two weeks. I highly recommend using these two recipes every day if possible, StomachClenz and BowelClenz.
DOSE: Take 2 scoops daily in a smoothie as your Breakfast and Lunch

DOSE: Take 10ml twice daily away from food.
Repeating some of these herbs in a liquid formulation, and adding a couple of extra anti-inflammatory, immune-supporting herbs in a liquid will help increase the effect of the powered herbs taken in a smoothie.
See the ColonEze Liquid Formulation Here
Get everything in one complete package, and save 25%. The Ultimate IBS and Crohn’s Program comes with everything you need for the full 1-month treatment program. Click Here to Find out more
Body Mind Healing And Irritable Bowel Syndrome
Meditation And Irritable Bowel Syndrome
Going back to the brain-gut connection, there is an important role for the nervous system to play in IBS. Meditation can play a major role here. One randomized controlled trial demonstrated that mindfulness training has a substantial therapeutic effect on bowel symptom severity, improves health-related quality of life, and reduces distress. (7)
Interestingly, changes in quality of life, psychological distress, and visceral anxiety were not significantly different between groups immediately after treatment but evidenced significantly greater improvements in the meditation group at the 3-month follow-up. (7)
This makes sense, as the effects of meditation are known to increase over time. Read more Here
Follow up Plan to Irritable Bowel Syndrome Treatment
I would recommend continuing with the dietary advice until IBS symptoms have been absent for over 3 months, preferably 6 months, then gradually introducing foods as you feel comfortable.
Long term it would be best to minimize the inflammatory, acid-forming foods mentioned and keep up the good food and herbs.
It is always good to complete a Herbal Detox at least once a year and you can also use our other herbal products to continue your journey.
I hope this article has been helpful and please share your comments if you also find success with our recommendations.
Many Blessings
Brett Elliott ®
Irritable Bowel Syndrome Solutions Free eBook
How Food & Herbs can Heal IBS. This eBook explains what can cause IBS and what you can do yourself to solve the problem at home.
Brett Elliott has helped over 100,000 people with his Herbal Health Programs
You’ll Learn:
- What are the statistics, symptoms and potential causes of IBS look like from a holistic perspective
- Understanding the gut-brain connection, and how mental and emotional states affect IBS
- What your Doctor would prescribe versus the natural solutions you can use at home, including specific herbs and foods
- What’s involved in Brett Elliott’s Herbal program for IBS and some success stories from other IBS sufferers